I haven’t posted an update about my shoulder rehab process since last April, which is when I returned fully back to work. Not really a coincidence!
As of today it has been one year since my surgery to repair my torn labrum and Hill-Sachs lesion. For anyone just now catching this blog, I dislocated my shoulder when I tripped on a sidewalk crack and fell while jogging early in the morning January 14, 2021. I have been working very hard all year to rehab my shoulder. I would say it’s about 95% recovered at this point. I’m hopeful that there is still some improvement to be seen.
It has been a challenge to regain the mobility and rebuild the strength at the same time. I’m happy to report that my range of motion is nearly 100%. Functional reach behind my back is still a little limited but good enough to fasten a bra behind my back or loop my belt around the back of my waist. My strength is also mostly back to normal. I am able to do all of my work activities, including manual therapy, that I would normally do. I don’t notice many functional limitations at home either and was even able to return to playing tennis with my family this summer.
The big issue is still that pesky scapulohumeral rhythm, especially when I reach forward and up overhead.
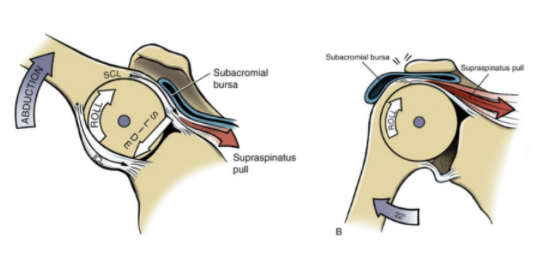
You can see that my scapula still wings a little bit as I raise my arms up and down. This is caused by the continued limited range of motion of the actual ball-and-socket joint of my shoulder. So more of the motion has to come from the shoulder blade moving excessively. This causes pinching of the soft tissue structures in the subacromial space because the humeral head does not glide downward as it rolls upward. As a result, these impinged structures cause pain. This pain is the biggest problem that is yet to resolve. I notice it the most at night because I still wake up several times a night in pain. If I spend too long in any sleeping position, it becomes painful and wakes me up. Happily, I am able to fall back asleep once I shift positions are rearrange myself. But my ultimate goal is to not wake up at night due to pain.
Even though it has been a full year since surgery, I feel like this is still slowly getting better. So there is still more room for improvement. I plan to continue working on loosening up the part of the joint capsule that is still restricting this movement, strengthening the scapular stabilizers, and working on neuromuscular control of the entire pattern. So I’m still hopeful it will get even closer to 100%.
I can’t round out this year of shoulder rehab without mentioning a little bit about my continuing work to recover mentally and emotionally from this injury as well. While tripping on a sidewalk crack might not seem all that traumatic or frightening, it really affected me. I still have anxiety about walking on the sidewalk, especially if it’s dark outside. I haven’t been able to run since this injury, and even watching other people run on the sidewalk gives me a lot of anxiety. (Run on the street, my friends!) I see this a lot with my patients. We develop avoidance behaviors, consciously or subconsciously, because something we did caused us pain. Sometimes it’s something big and traumatic, but sometimes it’s something little like hurting your back when you bent down to pick up a sock. So ever after you have fear that you’ll relive that pain whenever you pick up a sock. Or maybe you felt a tweak in your back and ignored it and a few days later that tweak turned into intense pain down your leg. So now every little tweak you feel sets off alarm bells. I began seeing a mental health counselor a couple of months ago to try to work through some of this because, while running is not my favorite thing to do, I would like to be able to do it if I feel like it without fear or dread. And as a PT I do need to be able to watch my patients run now and then to analyze a faulty gait pattern. I’m hopeful that working through some of these issues on the mental health side of the equation will also help me get to full recovery and prevent this incident from affecting what I can do for any reason, physical or mental.
Nothing is lost of course. This experience has given me more empathy for my patients, though that empathy has probably actually made me a tougher rather than an easier PT! (I’ve been through it, you can do it too!) Feeling the tightness and tension in my own shoulder has helped me understand the way some of the treatments I perform and prescribe for my patients feel, and how they can help. Prior to this injury all of my joints were so loose and hypermobile that I had a hard time understanding what restricted joint mobility feels like. Now I know!
I hope that in writing about my experience with this challenge I’ve helped people have a better understanding of injury, whether their own or someone else’s. I hope that reading this reminds you of the awesome resilience and general coolness of the human body and, of course, of the power of physical therapy!









