I’ve had my pre-op physical and got my COVID test, which was negative. I spoke to the nurse about pre-op instructions and to the all-important finance department! So I’m ready to go for surgery! While I’m waiting for surgery this coming Monday, I’ve been doing some things to keep myself moving within the limits that the damage to my shoulder will allow. There’s almost always something you can do, even when you are limited! Here are some of the things I’ve been working on:
1. Upper trapezius stretch- My neck gets tight from being in the sling and muscle guarding, which is when muscles near an injured area tighten protectively. This upper trap stretch helps.

2. Levator scapulae stretch- Same idea as the upper trap stretch but for the levator scapulae, which is more towards the back of the neck.

3. Backward shoulder rolls- Rolling the shoulders in backward circles helps with keeping the chest open, the scapulas (shoulder blades) mobile and the muscles around them working.
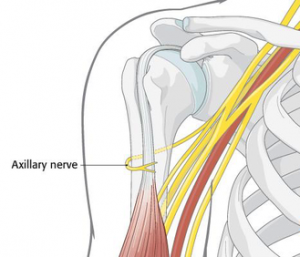
4. Shoulder isometrics- These can help prevent atrophy of the muscles from disuse. I’m also hoping this might help my axillary nerve, which was damaged by the dislocation, start to recover its communication with my deltoid muscle.
5. Shoulder passive range of motion- I’m using my left hand to support the right arm and gently raise it to about 90 degrees which is a relatively painfree, safe range of motion for me right now.
6. Supine alternating leg extension- I’m trying to keep my core strong using my legs for some dead bug exercises with the sling on to support my shoulder.
7. Pilates Arc stretch and roll up/roll down- This is my Pilates Arc, which I love. Sometimes I just lie back on it like this to stretch out my back, sometimes I do roll-ups from the position for some for core work.
8. Wrist and forearm range of motion- I’m moving my wrist and hand around in all directions so that it doesn’t get too stiff or atrophy from being in the sling.
9. Elbow range of motion/nerve glide- I’ve been doing this to try to keep my elbow from getting too stiff from being in the sling all the time.
10. Scapular retraction- I’m leaning forward letting my arm hang and pulling my scapula back and then relaxing it to let it go back to the starto try to keep my scapular stabilizing muscles from atrophying.
11. Pendulums- This is an exercise to gently move the shoulder joint in a painfree and passive way.
12. Stepper- I got this mini-stepper to try out before this injury happened and I’m so glad I did! It actually works really well for cardio and you can get a good burn going in your quads and glutes as well. I’ve been using this for short bouts a few times a day to try to keep up my cardio and leg strength.